|
Getting your Trinity Audio player ready...
|
ARTICLE/VIDEO from CampingCooks.com.
Lyme disease is an infectious condition caused by bacterial strains and spread by tick bites. While it can sometimes be misdiagnosed, there are about 365,000 known cases in the United States per year. If Lyme disease is diagnosed in its early stages, it can be cured with antibiotics. However, if left untreated, this infection can spread to other parts of the body, causing discomfort and even disability. In its late stages, antibiotics cannot cure the condition.
Awareness is key to avoiding long-term consequences of untreated Lyme disease. People who know the signs and symptoms of Lyme disease, and who recognize the tell-tale “bulls-eye” rash, and who understand the severity of a tick bite can protect themselves. If you suspect you or someone you love is suffering from Lyme disease, seek medical treatment before it’s too late.
If you spend time outdoors or in parts of the country where Lyme disease is common, take steps to protect yourself. Wear the right clothing, perform self-inspections after coming indoors, and avoid potential hot-spots where ticks are likely to be found. Clean up your camping kitchen when you’re finished eating so you don’t attract any host animals. If you find a tick on your body, remove it immediately and seek help from a qualified medical professional. Doing all these things could save you from a potentially devastating condition, which could affect you for the rest of your life.
Causes
There are three types of bacteria that can cause Lyme disease. Each type of bacteria is active in a different part of the world. While the bacteria can vary by location, transmittal of the disease is almost always caused by a bite from an infected tick. People are more at risk for Lyme disease if they spend time in places where ticks are likely to be found.
Ticks live outdoors, usually in wooded areas. If you go hunting, hiking, camping or do other activities in wooded areas, you are at a higher risk for contracting Lyme disease than people who do not. Your risk of contracting Lyme disease goes even higher if you spend time outdoors in a region where Lyme disease is more common.
In the United States, 95% of the cases of Lyme disease occur in just 28% of the states. The states where most of the cases of Lyme disease occur are: Delaware, Connecticut, Massachusetts, Maine, Minnesota, Maryland, New Jersey, New Hampshire, Pennsylvania, New York, Virginia, Rhode Island, Vermont and Wisconsin.
Still, Lyme disease has been found in every state but one. Even in low-risk states, anyone who goes outdoors, spends time in grass or natural debris could be at risk.

Borrelia burgdorferi
In the United States, the main cause of Lyme disease is a bacteria called Borrelia burgdorferi. This bacteria was named after Willy Burgdorfer, a scientist who first identified the strain in the latter half of the 20th century.
Borrelia burgdorferi is a type of corkscrew-shaped bacteria called spirochetes. These bacteria are slow to replicate. People who are infected with Lyme disease typically have a low number of bacteria in their blood stream, and detection can be difficult. Unlike many other types of bacteria, Borrelia burgdorferi can survive without iron. Instead, it requires a supply of manganese to survive. It is this unique adaptation that has lead some experts to suggest the condition could be treated by starving the bacteria of manganese.
This bacteria replicates in the midgut and is eventually released into the host’s bloodstream. Once this happens, the bacteria spreads throughout the body causing neurological and cardiovascular problems. Cases of Borrelia burgdorferi have increased dramatically in recent decades, and today, Lyme disease is considered a significant health problem in the United States. Lyme disease represents the most common tick-borne illness in the U.S.
Borrelia afzelii and Borrelia garinii
Like Lyme disease in the United States, cases of Borrelia afzelii and Borrelia garinii are on the rise in Europe. More than 360,000 cases of Lyme disease were reported in Europe between 1990 and 2010. The highest rates of the disease were found in Central Europe, specifically in Belarus, Croatia, Belgium, Russian Federation, Serbia, Norway, Bulgaria, Hungary, Finland, Slovakia, Czech Republic, Poland, Estonia, Slovenia and Lithuania.
Generally speaking, Borrelia afzelii and Borrelia garinii produce less severe forms of Lyme disease than Borrelia burgdorferi in the United States. The bacteria respond well to treatments, which can be particularly helpful during the early stages. Even in the later stages of the disease, Borrelia afzelii and Borrelia garinii can sometimes be treated with antibiotics. However, if too much tissue damage occurs before the antibiotics take effect, the treatment may not be fully effective.
Travelers to Europe should be aware of the risks, especially when spending time hiking. Ticks in Europe can be prevented using the same precautions one would use in the United States.
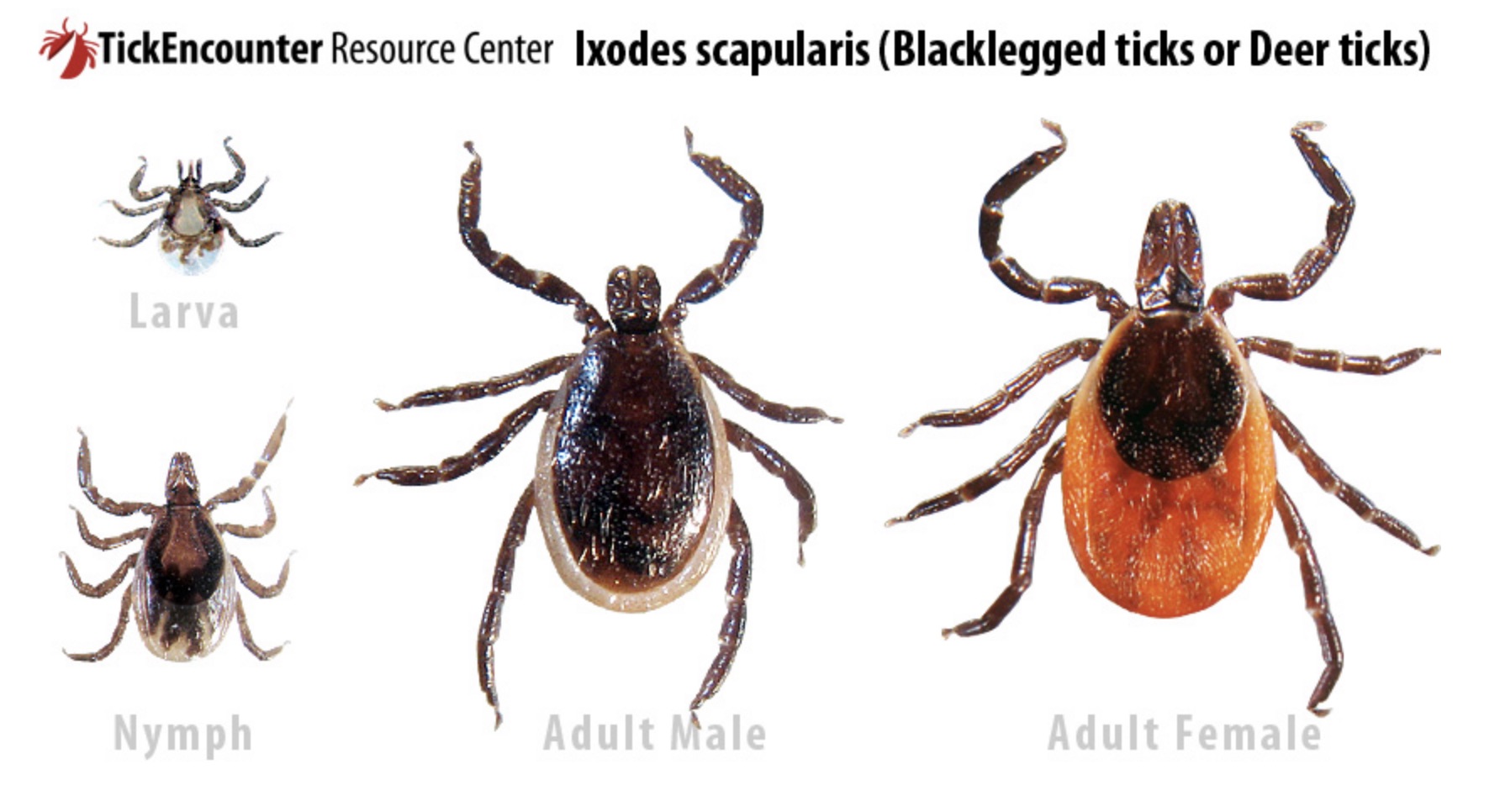
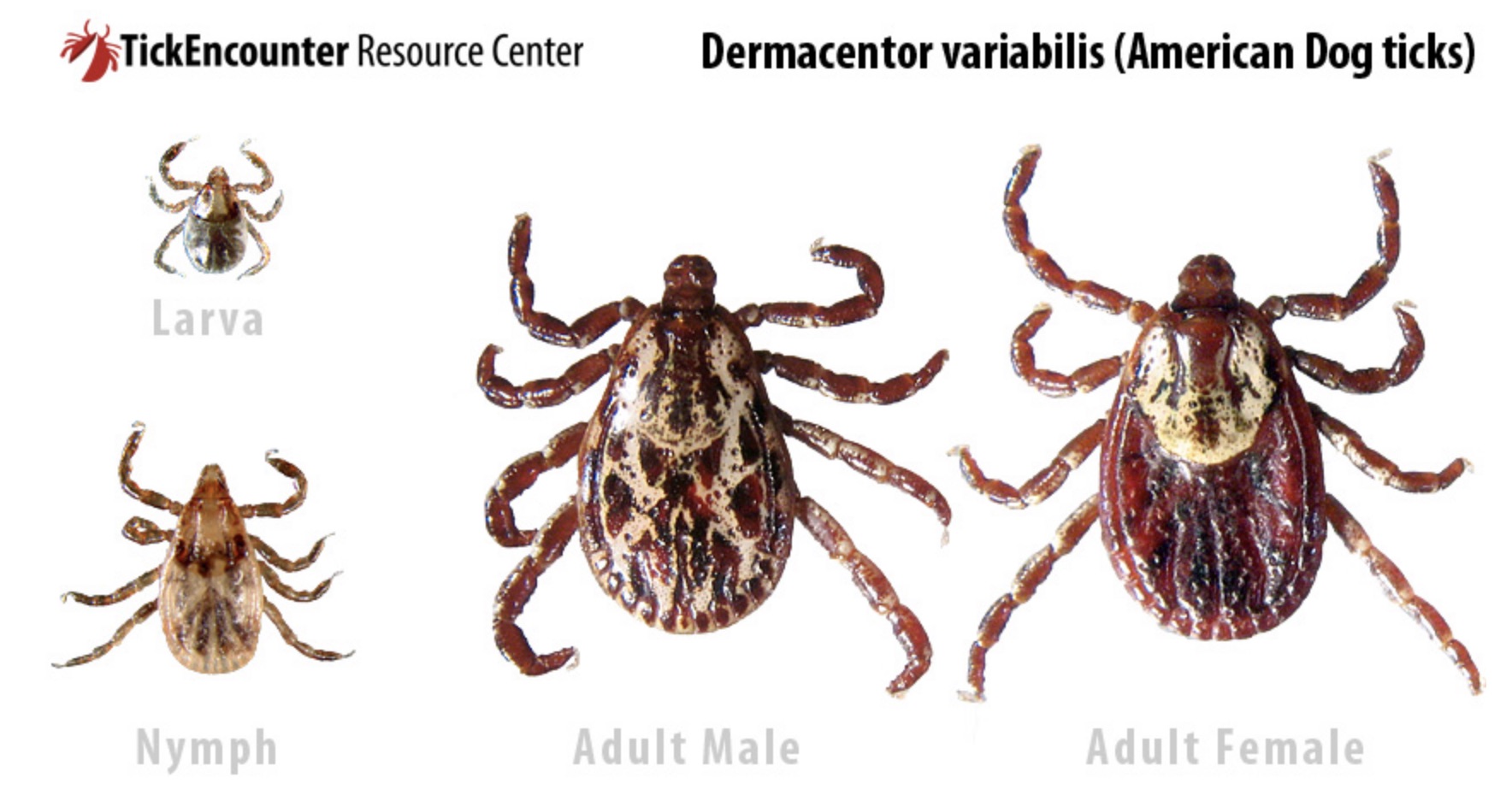
The Blacklegged Tick
Two types of ticks are responsible for spreading Lyme disease in the United States. On the west coast, this tick is called Western blacklegged tick, and on the East coast, it is the Eastern blacklegged tick. Eastern blacklegged ticks are more commonly known as deer ticks.
Lifecycle
Blacklegged ticks live between two and three years. They have four life stages: egg, larvae, nymph and adult. At each stage, ticks must have a blood meal from a host in order to progress to the next stage. While feeding, ticks may ingest bacteria from their host. This ingested bacteria can then be passed along from one host to the next host. This is how ticks spread Lyme disease.
Some pathogens can be passed from the tick to the host in as little as 15 minutes, while other pathogens take 24 hours or more. Lyme disease typically takes at least 24 hours, and in most cases, Lyme disease is not transmitted to the host until the tick has been feeding between 36 and 48 hours. People who are able to find and remove any ticks before the 24-hour mark are less likely to contract Lyme disease as a result of the tick bite.
How They Attach
Ticks are incapable of flying or leaping to their host. Instead, they wait for potential hosts at the end of tall grass or on organic debris in wooded areas. When the host walks past, whether it’s a person or an animal, the tick sticks out its legs and attempts to attach itself to the body of the host. When the tick makes contact and is able to grab on to the host, it crawls to a part of the body it finds desirable. Ticks do not often attach in the exact location where they grabbed on.
Ticks like to attach to the soft, thin skin found in the folds of the body, like on the back of the knees and in the armpits. They can also be found on top of the head. People who perform tick checks after spending time outdoors must be aware of tick hotspots, or they are unlikely to find a tick on their body.
Host Animals
Ticks generally get Lyme disease from host animals like the grey squirrel (found on the West coast) and the white-footed mouse (found on the East coast). In addition, ticks also get their food from animals like small mammals, birds and the white-tailed deer. This is one of the reasons why it’s important to keep a safe distance when handling an animal encounter in the wilderness. However, not all hosts pass bacteria along to ticks. In fact, when a tick feeds upon the Western Fence lizard, the bacteria inside the tick is destroyed by the lizard’s immune system.
Lyme disease is not the only bacteria ticks can get from their host animals, and it only takes one case of biting an infected host for the tick to become infected itself. In fact, ticks only need a few blood meals to live several years, so by the time a tick has passed along Lyme disease to a human, it may have only fed once or twice before.
Are There Other Ways to Get Lyme Disease?
Ticks are the primary source of Lyme disease in humans. However, it’s common for people to have questions about other potential ways to contract Lyme disease. For example:
Can You Get Lyme Disease from Another Person Who Has Lyme Disease?
You cannot get Lyme disease by kissing or touching someone who has been infected with the bacteria.
Can You Get Lyme Disease from a Blood Transfusion?
There is no evidence to suggest a person with Lyme disease can pass the condition to a blood recipient; however, people who have Lyme disease are asked not to donate blood until they have completed a course of antibiotics. If you have symptoms of Lyme disease, do not donate blood until you have spoken with a doctor and have been cleared for donation.
Can a Pregnant Mother Pass Lyme Disease Along to Her Child?
Pregnant women infected with Lyme disease who do not receive treatment for their condition may have a stillbirth pregnancy. In some cases, a stillbirth may not occur, but the placenta may become infected. Pregnant women who become infected with Lyme disease can generally complete a course of antibiotics without damaging the fetus. A woman who is infected with Lyme disease and who is breastfeeding their child may continue to breastfeed, as there have been no known cases of Lyme disease passing from mother to child via breast milk. If you are a pregnant woman who believes you may have Lyme disease, work with your doctor to receive safe treatment.
Can You Get Lyme Disease from an Infected Animal?
You may get Lyme disease if you come into contact with an animal playing host to a tick, as ticks that come into contact with your skin may transfer from the animal host to you. This is true of ticks on pets and on animals you choose to hunt. You cannot get Lyme disease from eating the meat of an animal that was infected with the bacteria that causes the condition.
Can You Get Lyme Disease Through the Bite of a Mosquito?
No, Lyme disease cannot be transmitted in this way.
Signs and Symptoms

Early Stage Symptoms
It is during this early stage the condition is most easily treated. Most often, the disease goes away when treated with antibiotics in its early stages.
The most obvious side effect of the tick bite is a warm, red area where the bite occurred. This rash occurs in as many as 80% of the people who are affected with the condition. Typically, the rash doesn’t appear until about 7 days after the bite first occurs. As this bite ages, the red spot may become clear in the center and larger overall, so that it resembles a “bull’s eye” shape. This shape may become as large as 12 inches across, or larger. This is a tell-tale sign of Lyme diseases. Anyone who sees this symptom should immediately go to a doctor for treatment.
Other early-stage symptoms of Lyme disease are flu-like and include fever, headache, joint aches, fatigue and chills.
Late Stage Symptoms
Late stage symptoms are also flu-like, with headaches and muscle stiffness. Patients may experience rashes in other parts of their body, and may experience joint pain and swelling. This is especially true around the knees and other large joints in the body.
Loss of muscle tone in the face, known as facial palsy, is another symptom of Lyme disease, as are heart palpitations, dizziness, shortness of breath, intermittent pain in the muscles and joints, inflammation of the brain and spinal cord, shooting pain, tingling in the hands and feet and nerve pain.
Erythema Migrans
The rash people experience when they get Lyme is called Erythema Migrans. This condition is not a reaction to getting a bite from a tick, as many people suspect, but is instead an outward manifestation of Lyme disease. This rash is so distinctive that many doctors will diagnose the condition based solely on the rash, but will follow up with blood tests to ensure the diagnosis is correct. This rash expands relatively quickly. Some people experience a rash that appears more bruise-like, with purple, blue or brown coloring, rather than red or red and yellow coloring.
Generally speaking, Erythema Migrans is not itchy or uncomfortable. However, if the rash does become itchy, it can be treated with a cold compress or with antihistamines, just like any other rash. The course of antibiotics that can be used to treat Lyme disease will also take care of the rash.
Erythema Migrans lasts for a few weeks in most people, although it can last months for some. If the disease progresses to late-stage Lyme disease, the patient may also experience new cases of Erythema Migrans.
Early Localized Disease
Lyme disease symptoms can begin hours, days or weeks after the initial tick bite, but typically symptoms begin one or two days after the first tick bite occurs. One of the first things most people notice when they’ve been infected is Erythema Migrans (bull’s eye rash described above) found in the same location where the tick bite occurred.
In addition to the rash, early localized disease can include flu-like symptoms such as fever and chills, sore throat, enlarged lymph nodes, vision changes, muscle aches, fatigue and headaches. Diagnosis at this stage is usually based on the presence of the rash and the coincidence of a trip to a wooded area or a location where ticks are known to be. At this stage, antibiotic treatment is effective against Lyme disease. Some people do not experience any symptoms during this stage.
Early Disseminated Lyme Disease
The second stage of Lyme disease is known as early disseminated Lyme disease or early disseminated infection. This stage can begin between one and four months from the initial tick bite. This second stage of Lyme disease occurs if the first stage is not caught and the disease is allowed to progress. At this stage, the condition begins to affect the nervous system, heart, skin and joints in the body. Symptoms include:
- Difficulty using muscles in the face
- Headaches
- Fainting spells
- Weakness, pain or numbness in the legs and arms
- Inability to concentrate
- Poor memory
- Circular rash on various parts of the body, including a circular rash at the site where the tick bit the patient
- Damage to the tissues in the eyes
- Problems with the joints, including swelling, especially around the knees
- Rapid heartbeat and other heart problems
Once the condition has spread to other parts of the body, it may be more difficult to detect. If your doctor suspects you have early disseminated Lyme disease, your doctor may recommend one or more of the following tests to diagnose.
- MRI of the brain
- Spinal tap
- Tests to examine the functioning of the heart
Successful treatment during the early disseminated stage is still possible, but if the condition is not treated before it progresses even further, long-term damage is possible.
Late Disseminated Lyme Disease
The final stage of Lyme disease is called late disseminated Lyme disease. During this stage, Lyme disease can cause damage to the brain, nerves and joints. This final and most serious stage of Lyme disease is characterized by a variety of symptoms, including:
- Feelings of fatigue
- Tingling or numbness in the back, feet and hands
- Arthritis in the knee, or fluid build up and redness in the joints
- Difficulty speaking
- Heart problems, especially pericarditis
- Inability to control the muscles in the face
- Difficulty remembering things
- Insomnia
- Trouble with speech
Some symptoms of late disseminated Lyme disease can be treated, but total eradication of the disease may not be possible once it reaches the later stages.
Prevention

Parents of young children who spend time outdoors should also be aware of these methods and should encourage their own children to practice prevention whenever possible. The following methods can prevent you from coming into contact with infected ticks.
Protect Yourself From Tick Bites
When spending time outdoors, especially in grassy or wooded areas, use these methods to repel ticks. Ticks can be found in almost any outdoor location, including backyards, so don’t think you’re safe from a tick bite just because you’re not engaging in a strenuous outdoor activity. Even gardening and mowing your lawn can expose you to potentially harmful ticks.
- Walk down the middle of trails, avoiding high grass on either side of the trail
- Use standard insect repellant on exposed skin
- Wear light-colored clothes to make it easy to see a tick if one should attach itself to you
- Wear long pants and tuck them into your socks to make it impossible for ticks to reach your skin
- Tape up holes in your pants or gaps in your clothing
- Wear hats
- Stay away from bushes, shrubs, debris and tall grass when walking around outside
You can also use permethrin insect repellant on clothing. Permethrin stays on clothes through one or sometimes more washings. You can also buy clothes treated with insect repellant, which can last longer than repellant you put on after buying the clothing.
Perform Daily Tick Checks
After spending time outside in an area where ticks are known to be found, perform a “tick check” to look for ticks in their favorite places. Do not expect to feel a tick crawling on your skin or biting you. The only way to know for certain that you do not have a tick on your body is to perform a check. Look for ticks in the following areas:
- Inside the ears
- Around the outside of the ears
- Under the arms
- Back of the knees
- Inside the belly button
- Around the waist
- On the head, inside the hair
- Between the legs
If you spent time outside with a young child or pet, check your young child and pet for ticks as well. Pets tend to get ticks in the same sensitive areas as people, including the space between their legs and their body, the area around and inside their ears, the folds of their neck, and so on. If your pet brings in a tick, the tick could eventually transfer from your pet to you. Feel for a hard bump.
Shortly after biting, ticks become small. They get larger as they ingest more blood. You may not feel a tick at first, but could feel a tick later after it has fed on blood. Performing multiple tick checks is wise.
Remove Attached Ticks Quickly and Correctly
There are many myths, most incorrect, about how to remove a tick from the body. To remove a tick, use tweezers with a fine point to grasp the tick. Place the tweezers as close to your body as possible. Pull the tick up and away. Pull the tick slowly. When done, clean the area with rubbing alcohol. If you have trouble removing the tick, contact a physician for help.
Ticks must be removed from pets in the same way, using the same methods, that they are to be removed from your own body. If you are unable to safely remove the tick from your pet’s body, contact your pet’s veterinarian.
Do not attempt to burn the tick, use ice to freeze the tick, or attempt to remove the tick with your bare fingers. Do not twist the tick, or crush it against your body.
Create a Tick-Safe Zone Through Landscaping
If you’re a homeowner, you can deter many ticks from your yard by maintaining your property and making your yard less attractive to ticks. Keep your grass mowed and leaves raked. Use a weed wacker or edger to remove tall grasses from the edge of your yard. If your yard is adjacent to a wooded area, dig up the grass that borders the wooded area, and lay down mulch to prevent ticks from wandering onto your property.
Keep playground equipment surrounded by mulch. If installing playground equipment on your property, install it in a sunny, dry part of the yard. Do not install playground equipment near wooded areas or the edge of your yard.
If you store wood on your property, stack it neatly and keep it dry, to prevent tick-carrying rodents from entering your property. Remove any trash or debris from your lawn, including mattresses, furniture or rolls of carpet.
Tick pesticides, known as acaricides, can also help keep your yard tick-free. Spray your yard with acaricides, but do not rely solely on this form of lawn care to prevent ticks. When spraying your yard with acaricides, follow the manufacturer’s instructions. Store acaricides in a dark, cool, dry location.
Finally, keep deer and mice off your property. Install a fence to prevent deer from wandering onto your lawn, and work with a pest control company to keep mice away from your home. If you’re camping, a smell-proof bear canister can help prevent hugry animals from wandering onto your campsite. For that same reason, don’t throw any food waste into collapsible trash cans when camping/ These animals can bring ticks with them, and may thwart any efforts you make to keep ticks away.
Vaccination?
Currently, there are no vaccines to protect people from Lyme disease. In the late 1990’s and early 2000’s, a vaccine called LYMErix was made available on the market and was given to a limited number of recipients. However, LYMErix eventually proved to have side effects. (Namely, it was associated with joint pain.) The potential side effects combined with a growing distrust of vaccines in general lead to a poor market performance, and the vaccine was eventually discontinued.
Today, companies are once again searching for a potential vaccine against Lyme disease. Many experts expect a breakthrough in Lyme disease treatment and prevention will become available sometime in the relatively near future. People who live in high-risk areas for Lyme disease, and people who participate in high-risk activities, should work with their doctor to ensure they are able to obtain a vaccine as soon as a safe product becomes available.
It’s worth noting there are multiple Lyme disease vaccines for dogs. These vaccines are available for sale now and can be obtained through a veterinarian. If you have a pet and you live in a high-risk area for Lyme disease, work with your pet’s veterinarian to obtain the vaccine (if appropriate). Protecting your pet from Lyme disease will not protect you from tick bites or Lyme disease.
Diagnosis
Most people do not recognize the signs of Lyme disease when they appear. Some wait for the symptoms to go away, and when the symptoms do, they believe their condition has resolved itself. What they do not know is Lyme disease comes and goes in phases, and the disappearance of one stage will only lead to the next.
If you are showing signs of potential Lyme disease, see a doctor, even if the symptoms seem to go away. If the condition is caused by Lyme disease, then diagnosis is critical. Without proper diagnosis and care, your disease will progress and you could eventually suffer from a long-term condition, which is difficult to manage and uncurable even with antibiotics.
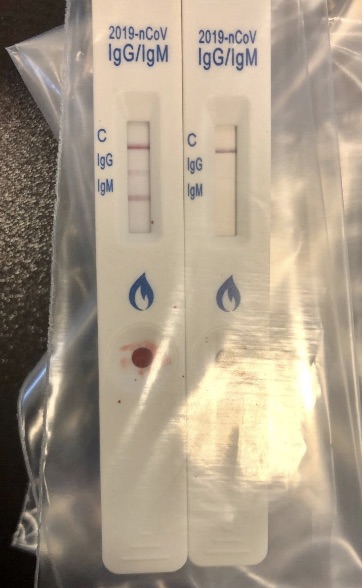
Lab Testing
Lab testing is currently a two-step process requiring a blood sample in order to complete. The first step, the enzyme-linked immunosorbent assay (ELISA) test, detects antibodies to Borrelia burgdorferi. However, test results can sometimes produce a false-positive, so typically if the test is performed and the results indicate presence of antibodies, then the second step must also be performed. If the results of the first step are negative, then the second step is not necessary.
The second step is known as the Western blot test. The Western blot test detects antibodies of proteins from Borrelia burgdorferi. If Western blot test results are also positive, the patient can be definitively said to have Lyme disease. In the early stages of Lyme disease, tests may not produce positive results for the disease. However, patients who have the rash and who live in areas where ticks are known to transmit Lyme disease may be diagnosed and treated without further testing.
Imaging
In the later stages of Lyme disease, damage done to the body can be evidence of the presence of the disease. Some types of imaging, like MRI scans of the brain, can be used to show Lyme disease is present in the body. The types of imaging that can be helpful in the later stages of the disease varies. Work with your doctor to find the right imaging test for your condition.
Treatment

In some cases, intravenous antibiotics are used to help patients. This is more common for patients suffering from cardiac or central nervous system involvement. After a successful course of intravenous antibiotics, the patient may eventually switch to oral antibiotics. This type of treatment can take as long as one month to complete.
New Research
Lyme disease has been around for thousands of years. In fact, not long ago, bacteria linked to Lyme disease was discovered in a mummy more than 5,000 years old. However, Lyme disease was first recognized as a condition in the 1970’s, in connection with tick bites in the area of Old Lyme, Connecticut. What once was frequently misdiagnosed as arthritis was eventually discovered to be a separate disease.
Treatments were developed throughout the 1970s and 1980s as new research uncovered information about the bacteria. Today, cases of Lyme disease are increasing all the time. Over 300,000 cases of Lyme disease are diagnosed each year. What was once a phenomenon on the East coast of the United States only has now spread to all 50 of the United States except for Hawaii. There continues to be no fully effective treatment for late stage Lyme disease.
As this infection continues to grow and reach new parts of the United States, research will continue to play a big role in treatment and prevention.
Borrelia Miyamotoi and Borellia Mayonii
Borrelia miyamotoi is a newly discovered tick-borne parasite, shaped like a spirochete, which causes Lyme-like symptoms in humans. The first case of infection was diagnosed in 2011, though some studies show the bacteria can be linked to ticks all the way back to 1995. Cases of human infection have been reported in the United States, New Jersey and Massachusetts.
Symptoms of infection include fatigue, joint and muscle pain, headache, fever, loss of appetite, memory loss, disorientation, neurological problems and lack of coordination. Treatments prescribed for Lyme disease have shown to be effective against this condition.
In addition, Borrelia mayonii is another new bacteria shown to cause Lyme disease in North America. This bacteria was discovered in 2013 by the Mayo Clinic. Borrelia mayonii was discovered in blacklegged ticks in the Upper Midwest, including Wisconsin and Minnesota. Symptoms of infection include headache, rash, fever, neck pain, large rashes, nausea and vomiting. This is slightly different from symptoms of infection from Borrelia burgdorferi because typical Borrelia burgdorferi infections do not usually include nausea and vomiting. Borrelia mayonii also produces a higher concentration of bacteria in the blood.
The same testing that can diagnose Lyme disease can also be used to diagnose infection from Borrelia mayonii. As in the case of Lyme disease caused by Borrelia burgdorferi, a diagnosis may be made without testing at all if the case occurs in an area where infection is known to occur and the rash can be verified by the physician.
Borrelia mayonii can be treated with doxycycline and some other forms of antibiotics.
People can protect themselves from this new bacteria using the same precautions they would use to protect themselves from Borrelia burgdorferi. By wearing proper clothing, long pants, light colors and using insect repellent, people can avoid tick bites and potentially avoid infection from Borrelia mayonii or Borrelia miyamotoi. Tick checks after spending time outdoors can also help.
Red Meat Allergy
Tick borne illnesses are not limited to Lyme disease. The blacklegged tick is known to cause Anaplasmosis and Babesiosis, among other conditions. Perhaps one of the most unusual conditions caused by a bite from a blacklegged tick is an allergy to a carbohydrate, called galactose-alpha-1,3-galactose (or alpha-gal), found in red meat.
Diagnosis of the alpha-gal allergy can be very challenging because the condition may not occur until months after the tick bite. In addition, the allergic reaction to the carbohydrate may not occur until approximately 4 to 8 hours after the meat was consumed. The random nature of the allergy can make linking the allergy to its trigger very daunting. Many people take a long time to finally discover the exact cause of their discomfort.
Most people who develop an allergy to alpha-gal do develop some kind of respiratory problems in response to consumption of red meat. Others experience discomfort in the gut, or skin reactions.
Why Does Red Meat Allergy Occur?
Scientists are not quite sure what about tick bites causes red meat allergy to occur. However, some theorize when the tick bites the human, alpha-gal carbohydrates may be transferred from the tick to the host. In most cases, the immune response from the human will wipe out the alpha-gal, just as it would wipe out other unrecognized organisms. However, in some cases, the immune response may misfire, and the allergy occurs.
Is There a Cure?
Some people lose their alpha-gal allergy over time. Others have the allergy for the rest of their lives. Those who have the most severe reactions may even lose the ability to drink milk or eat gelatin, which both contain alpha-gal. The only way to manage this allergy is by avoiding red meat until it is no longer an allergy trigger, if that time ever comes.
For some people, this could involve a serious lifestyle change. Although the condition is rare, it’s important to be aware of the possibility of this condition occuring.
Protect Yourself from Lyme Disease

If you are bitten by a tick, take it seriously. Remove any ticks immediately upon discovering the tick on your body. Talk to your doctor, even if you are able to remove the tick within minutes of the bite. Watch for symptoms in the days and weeks after your tick bite occurs. Remember Lyme disease can be hard to detect in the early stages, and your first sign of an infection may be the tell-tale rash. Lyme disease left untreated can lead to additional and more severe problems, so get help as soon as you notice the warning signs. By taking these precautions, you can protect yourself from a potentially devastating disease.