|
Getting your Trinity Audio player ready...
|
OWN VOICE. ~ InPerspective by Bruce Laird and Gregg Dieguez —
The Good News is that vaccines are still strong protection against severe illness and death from COVID-19. The Bad News is that the Delta Variant is escaping our vaccine protection according to a new study which shows our best vaccines fading in effectiveness vs. the Delta Variant.
Footnotes: to use, click the bracketed number and then click your browser Back button to return to the text where you were reading.
Images: Click to enlarge for improved readability in a new window.
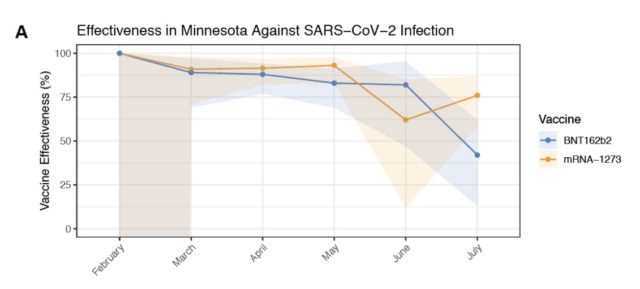
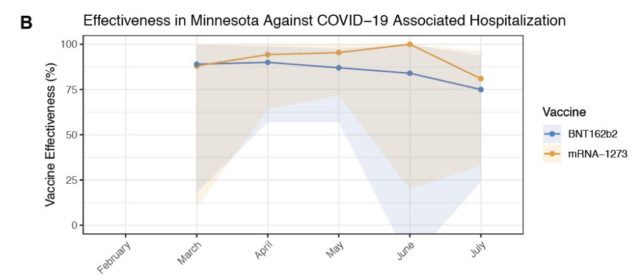
A report this week out of the Mayo Clinic in Minnesota based on 50,000 patients showed the effectiveness of the Pfizer vaccine declining to 42% versus the Delta variant, and Moderna’s to 76%. (chart above^) We believe the J&J vaccine is likely 15% or less effective. Why? And what does it mean going forward?
1. Vaccines still protect against severe illness and death from COVID-19.
The evidence for this remains overwhelming, including the fact that 99% of recent deaths and hospitalizations (since Delta took over) come from UNvaccinated persons. Think of your vaccine as a life preserver – you may get wet and cold, but you will survive long enough to be rescued.
2. Vaccines are not perfect
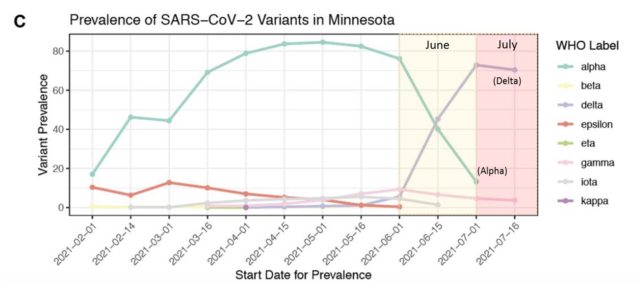
We knew this from the beginning, because 95% is not 100%, and in fact those numbers were estimates for a range of underlying probabilities from 88 to 98%, for even the best (mRNA) vaccines. And many people were getting Astra Zeneca, J&J, or worse, the Chinese and Russian vaccines. What is news this week is that our BEST vaccines, Pfizer and Moderna, have faded to 42% and 76% efficacy against the Delta virus, which is now the dominant strain (chart at right >). And we suspect that J&J is no better than 15% effective with a single shot.
WHY and HOW did this happen?
For two reasons:
A. First, all vaccines fade in effectiveness over time, as we discussed last week. The antibodies produced by your immune system in response to the vaccine will fade over time. They will also train your immune system (memory B cells and T-cells) to produce more antibodies, faster, the next time they spot a similar virus. Click Here to read details…
B. Secondly, the SARS-CoV-2 virus is evolving every minute, with trillions of experiments being conducted in host human bodies every day, and the successful experiments becoming new strains, or variants, which we detect if we do genomic testing on a patient. The successful experiments become more transmissible and/or more deadly, and they evolve to escape our immune responses and our vaccines. This drop in vaccine effectiveness was recently forecast by an important paper, and confirmed by the Mayo Clinic paper mentioned above. Click Here to read details…
We can combine these two factors: waning immunity from the vaccine, and the degree of ‘escape’ from protection caused by a viral variant, into an assessment of the likely effectiveness of a vaccine. Click Here to read details… And that process, described below, shows that vaccine effectiveness after 6 months is too low for any of the current vaccines to create Herd Immunity for the Delta variant. We need a vaccine efficacy of about 90%, possibly higher, to stop the Delta variant Click Here to read details…
3. We’re going to need booster shots
Extra shots of the vaccines will re-stimulate our bodies’ immune systems and re-strengthen protections. Click Here to read details… They will prevent a lot of severe illness and death, and help stamp out the virus, if we all take them. Click Here to read details…
4. We’re not going to be safe until everyone, nationally, and then worldwide, is vaccinated.
The Delta variant was first discovered in India. The Lambda variant, headed our way in increasing numbers was first identified in Peru. There are over 3,800 strains of SARS-CoV-2 (the virus causing COVID-19) that we know of today, and the number will continue to evolve and grow unless or until we wipe it out like Smallpox and keep it wiped out with continued vaccinations (unlike Measles, which has made a comeback thanks to Anti-vaxxers). We can debate how many doses of what vaccines go to what countries in what sequence, but as long as there are people traveling and shipping between countries this virus will continue until we vaccinate the entire planet, and now maybe deer.
5. Masking and other public health measures will still be required, likely for years.
Since the vaccines are not perfect, there is always a chance people – even vaccinated people – can pass it along and it can “break through” their immune protections and cause an infection. The evidence for masking as viable protection is overwhelming, and that protection will be needed because even vaccinated people can be harmed. And that harm goes beyond severe illness or death…
A recent Israeli study of health care workers showed that even health care workers – masked and gowned, but regularly exposed to the virus – contracted breakthrough cases, and 19% of those cases resulted in Long COVID. We won’t know for years how long “Long” is, and how much damage to the lungs, heart, and brain is being done, and whether that damage is permanent or reparable. Meanwhile, we need Public Health precautions: vaccines, masks, distancing, avoiding superspreader events, testing, quarantine, and contact tracing – until COVID-19 is an isolated and easily contained illness.
There is MUCH more that could be said about our governance, and willingness to act on the parts of our constitution which “insure domestic tranquility, provide for the common defence, promote the general Welfare, and secure the Blessings of Liberty”, about the need for a society based on facts and truth as much as ideology, but let us leave you with one thought from a famous forebear:
We must, indeed, all hang together or, most assuredly, we shall all hang separately.”
– Benjamin Franklin
DETAILED EXPLANATIONS:
How Immunity Fades and Responds As Needed
Waning immunity is an expected part of the immune system’s gradually declining response over months and years following a natural infection, or after getting a vaccine. Vaccination triggers a large initial increase in the number of immune cells (both B cells and T cells). When the presence of a new pathogen (or vaccine) is detected, B cells are programmed in the lymph nodes to produce a variety of antibodies (Abs) and other molecules that target the virus. T cells are also ramped up to fight the virus in other ways. Over months and years following vaccination, the immune system will gradually slow its production of Abs and T cells that target this particular virus, as long as they are not needed. But a small assortment of memory B cells and T cells remains to provide surveillance of the body for signs of reinfection by the virus. If the body is reinfected, those memory cells are capable of ramping up more quickly than before, and even have the ability to mutate in ways that produce evolved versions of the original antibodies.
If you want more detailed science on vaccines and immunology, the standard reference is: “Plotkin’s Vaccines,” by Stanley Plotkin, Walter Orenstein, Paul Offit, and Kathryn M. Edwards, 7th edition. 6 Jun 2017. Conveniently, Chapter 2 from the book, “Vaccine Immunology” by Claire-Ann Siegrist, is available as a pdf on the WHO website:
https://www.who.int/immunization/documents/Elsevier_Vaccine_immunology.pdf
It’s pretty heavy reading, so here are two good lay articles that are easier. The first is: Katherine Wu, “The Body Is Far From Helpless Against Coronavirus Variants.” The Atlantic, 12 Feb 2021. From Katherine’s article:
“The biggest misconception is these immune responses are all or none,” Marc Jenkins, an immunologist at the University of Minnesota, told me. Importantly, the vaccines still seem to largely ward off severe disease and death—a hint that residual antibodies and T cells are still making a dent, Jenkins said. (Scientists also expect that these vaccines will undergo mild to moderate dips in efficacy against the variants, based on early data from laboratory experiments.)
The protection offered by vaccines doesn’t need to be bulletproof to have an effect. “Even if vaccination does not prevent infection, the B cells and T cells will prevent severe disease and bolster immunity, which is incredibly important,” Smita Iyer, an immunologist at UC Davis, told me.
This article talks about vaccines waning in the context of boosters. See: Ewen Callaway, “COVID vaccine boosters: the most important questions.” Nature, 5 Aug 2021. From the article:
Scientists typically look at antibody levels, or titers, as a proxy for how well a vaccine has worked. These usually spike along with a surge in short-lived B cells and then fall as the cells dwindle. Memory B cells and bone-marrow plasma cells continue to churn out antibodies, but at reduced levels, for decades. That’s expected. “There isn’t a vaccine where you don’t see a drop over time in antibody titres and T-cell titres,” says Ahmed, [Rafi Ahmed, an immunologist at Emory University]. “There is always a drop.”
A booster does several things to these cells, says Ali Ellebedy, a B-cell immunologist at Washington University in St. Louis, Missouri. It causes antibody-making B cells to multiply, elevating the levels of antibodies against the pathogen once more. In time, their numbers will dwindle again, but the pool of memory B cells left behind will be larger than before, leading to a faster, stronger response to subsequent exposures. Boosters also promote a process called affinity maturation, in which ‘engaged’ B cells — those that have been triggered by the vaccine — travel to the lymph nodes. Here, they gain mutations, making the antibodies they produce bind to pathogens more strongly, potentially enhancing their potency.
Numbers of memory B cells and antibody levels will eventually plateau with repeated boosting (or reinfection), but it is unlikely that such levels have been reached in people who have had the recommended regimen of COVID-19 vaccine or a previous infection, says Ellebedy. A booster shot should elicit stronger immune responses, says Ahmed. “It will boost.”
Booster Shots Are On The Way:
The CDC’s Advisory Committee on Immunization Practices (ACIP) will meet this Friday, 13 Aug 2021.
Topics on the Aug 9 draft agenda include:
– Updates on [benefits of] additional doses in immunocompromised individuals (Dr. Kathleen Dooling)
– Considerations for booster doses of COVID-19 vaccines (Dr. Sara Oliver)
In related news, there is reporting by ABC News7 that supplemental shots will be given at SF General Hospital, but only for people who got the Janssen (J&J) vaccine. Recipients will get one of the mRNA vaccines. From the article:
Even though the CDC is not recommending a booster shot at this time, Zuckerberg San Francisco General Hospital and San Francisco’s Department of Public Health have decided to allow an extra coronavirus vaccine for people who got the single-dose Johnson & Johnson vaccine. The new dosing allowance seems to be unique to San Francisco. The hospital’s chief of staff does not know of any similar guidance elsewhere at this time.
The NIH announced yesterday that a trial of supplemental doses will begin for immune suppressed kidney transplant patients. See: “NIH launches study of third COVID-19 vaccine dose in kidney transplant recipients.” NIH News Release, 7 Aiug 2021. From the release:
The pilot study, called COVID Protection After Transplant (CPAT), is being conducted at Johns Hopkins University in Baltimore under the leadership of Dorry Segev, M.D., Ph.D. Dr. Segev is the Marjory K. and Thomas Pozefsky professor of surgery and epidemiology, associate vice chair of the department of surgery, and director of the Epidemiology Research Group in Organ Transplantation at Johns Hopkins University.
The lifelong immunosuppressive therapy that organ transplant recipients must take to prevent organ rejection blunts their immune response to both pathogens and vaccines. Research has shown that many organ transplant recipients do not develop antibodies against SARS-CoV-2, the virus that causes COVID-19, after receiving an authorized COVID-19 vaccine regimen. The purpose of the new study is to determine whether a third dose of one of the mRNA COVID-19 vaccines could overcome this problem for at least some kidney transplant recipients. This is particularly important because this population has a high prevalence of conditions that are risk factors for severe COVID-19, such as cardiovascular disease and diabetes.
Estimating Vaccine Effectiveness Over Time
At the end of July, Pfizer reported a 12% drop in effectiveness of their mRNA vaccine after 6 months. This was based on data from an ongoing observational study of participants in their phase 3 clinical trials. See: Stephen J. Thomas, et al, Kathrin U. Jansen, and the C4591001 Clinical Trial Group, “Six Month Safety and Efficacy of the BNT162b2 mRNA COVID-19 Vaccine.” medRxiv, 28 Jul 2021.
The effectiveness of the standard two dose regimen against infection (all cases) declined from a peak of 96% (reached at two months post dose 2) to 84%, by six months post dose 2.
This preprint article has observational data from Pfizer’s ongoing study of adults who participated in their phase 3 clinical trial. The time period covered is out to six months post dose 2. Pfizer’s phase 3 trials originally enrolled 44,000+ participants, split between vaccine and placebo groups. Participants were enrolled in six countries. Counting both vaccine and placebo groups (almost all of whom later got shots), the numbers of participants were: Argentina 5,764 (13.1%); Brazil 2,900 (6.6%); Germany 499 (1.1%); South Africa 800 (1.8%); Turkey 498 (1.1%); and USA 33,586 (76.3).
The median age of all participants was 51 years, with 60% in the age 16-55 cohort, and 40% over age 55. After the FDA granted EUA for the vaccine back in Dec 2020, Pfizer offered the vaccine to those in the placebo group, and has since continued to follow both groups. At the 31 Mar 2021 cutoff point for this report, there were still 20,334 participants from the original vaccinated group, and 20,794 from the original placebo group who chose to be vaccinated and followed, so the reported results are based on large N data.
From the preprint:
Efficacy peaked at 96.2% during the interval from 7 days to <2 months post-dose 2, and declined gradually to 83.7% from 4 months post-dose 2 to the data cut-off, an average decline of ~6% every 2 months.
Ongoing follow-up is needed to understand persistence of the vaccine effect over time, the need for booster dosing, and timing of such a dose. Most participants who initially received placebo have now been immunized with Pfizer’s BNT162b2, ending the placebo-controlled part of the study. Nevertheless, ongoing observation of participants through up to 2 years in this study, together with real-world effectiveness data, will determine whether a booster is likely to be beneficial after a longer interval. Booster trials to evaluate safety and immunogenicity of BNT162b2 are underway to prepare for this possibility.
This observed decline in effectiveness doesn’t tell us anything about possible reductions in efficacy due to vaccine escape by recent variants, particularly Delta, because the study period ended at the end of March, 2021 – before Delta became significantly prevalent in any of the six countries where participants were enrolled, particularly the US.
Moderna and J&J have not yet published comparable data on antibody persistence from their extended observational studies. But back in April, Moderna put out a press release claiming their average efficacy against all cases over the 6 months after dose 2 was 90%, comparable to Pfizer’s average of 91%, as reported in the above preprint.
More bad news: studies show new variants escape from vaccines
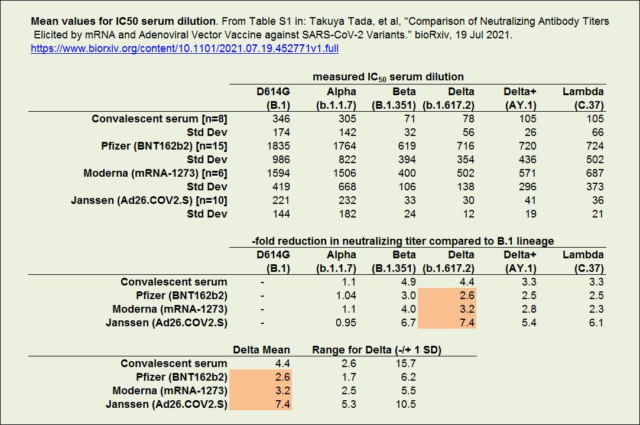
There is a recent paper that estimates, for those vaxed with Pfizer or Moderna, a roughly 3-fold reduction in neutralizing Ab titer when their blood samples are challenged with a Delta pseudotyped virus, compared to the titer when challenged with the older Wuhan B.1 lineage (with D614G mutation). The reduction is significantly greater for samples from those vaxed with Janssen (J&J) – at least 5-fold. The paper also measured this reduced neutralizing power for variants Alpha, Beta, Delta plus, and Lambda. See: Takuya Tada, et al, “Comparison of Neutralizing Antibody Titers Elicited by mRNA and Adenoviral Vector Vaccine against SARS-CoV-2 Variants.” bioRxiv, 19 Jul 2021.
These study results are based on a small number of samples, with large ranges of measured titers, and therefore large standard deviations (SDs) for mean estimates. But there are other titer studies that tend to confirm at least some of these values. At right is some of the data from the Tada, et al paper:
What I take from these values is that blood samples from those vaccinated with an mRNA vaccine experience an average 3-fold reduction in neutralizing titer against Delta, compared to the older Wuhan strain. For samples from those vaxed with the Janssen vaccine, the average reduction is significantly higher. I’ll be generous and say that it is 5-fold.
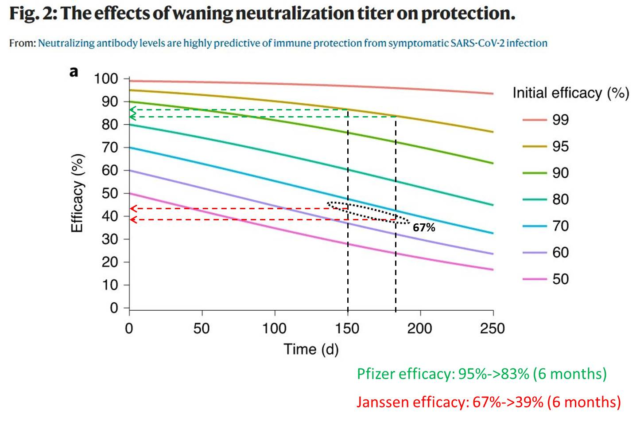
We can plug these estimates of 3-fold and 5-fold reduction into the empirical model that is described in this paper: David S. Khoury, et al, “Neutralizing antibody levels are highly predictive of immune protection from symptomatic SARS-CoV-2 infection.” Nature Medicine, 17 May 2021.
The paper is generating some buzz because it is one of the first to propose a quantitative relationship between something that can be measured from a vaccinated person’s blood sample (neutralizing titer), and how protected that person is likely to be from infection by a particular SARS-2 variant. They didn’t actually do human trial experiments, which would have ethics problems; so their model is using vaccine efficacy as a proxy for probability of infection. Using their predictive model, the authors have generated curves that predict the reduction in net vaccine efficacy, from both waning immunity and immune escape by variants.
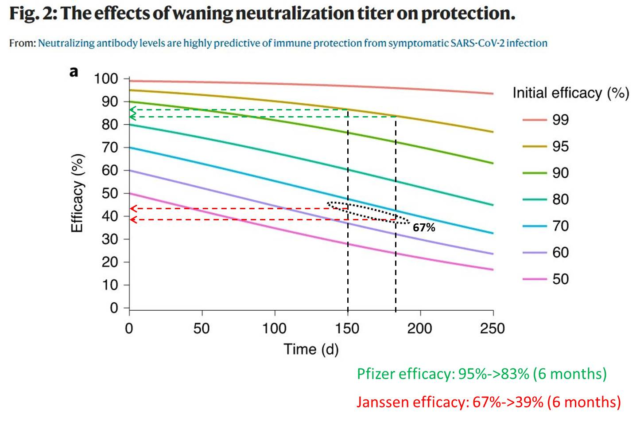
On the waning immunity front, their model agrees pretty well with Pfizer’s observational study. At right is figure 2 from the paper, where I have added in the dashed green lines to show what their model predicts for reduction in efficacy after 150 and 180 days, for a vaccine like Pfizer’s that starts off at 95% efficacy. After 180 days, efficacy is predicted to drop to about 83%. I have also shown the trajectories for the Janssen vaccine, with dashed red lines. Janssen’s initial efficacy as measured from clinical trials was an average of about 67%. This model predicts that after 6 months, that efficacy against the original Wuhan B.1 strain will drop to about 39%.
How to Estimate Efficacy Loss due to both time and new variants
The Khoury paper also shows the predicted reduction in efficacy due to variant escape, as measured by the reduction in neutralizing antibody titer. Using data collected in other serological studies, the authors got a bunch of antibody titer measurements from people who had been vaccinated by one of 7 different vaccines, plus those who had recovered from a natural infection (convalescent plasma). They did a regression that fits a logistics curve to the reported ranges of efficacy for those 7 vaccines, against the neutralizing titers observed in people who had received those vaccines, expressed as -fold increase over those with convalescent serum only. This is the red curve with shaded red confidence limits shown below:

With regard to new variants escaping the vaccine protection, the authors make the statement “For variants, 5-fold lower neutralizing titer is predicted to reduce efficacy from 95% to 77% in high efficacy vaccine, or from 70% to 32% for lower efficacy vaccine.” Here’s how to understand that, using their model, as represented in the figure at left. We know that clinical trials of people who have been fully vaxed with mRNA-1273 (Moderna) have demonstrated ~95% efficacy against the original Wuhan strain, so we find that point on the red curve, and drop down to the x-axis (a log scale, which is hard to interpolate), where we see that, on average, antibodies from these people are expected to show an approximately 3.2-fold higher mean neutralization level than antibodies in convalescent plasma.
Now suppose that antibodies from these people are tested against a particular NEW variant, like Delta, and the test shows a 5-fold reduction in neutralizing titer. That means that the neutralization level against that variant is 1/5 of 3.2-fold, or 0.64-fold. So, we move left to 0.64 on the x-axis and go back up to the red curve. The corresponding efficacy is ~77%. This is why the authors say their model predicts that this new variant would reduce effectiveness of a high efficacy vaccine like Moderna’s from 95% to 77%. If we apply their model to a lower efficacy vaccine that has demonstrated only 70% efficacy against the Wuhan strain, we find that a 5-fold reduction in neutralizing titer with a new variant would be predicted to reduce efficacy to only 32%.
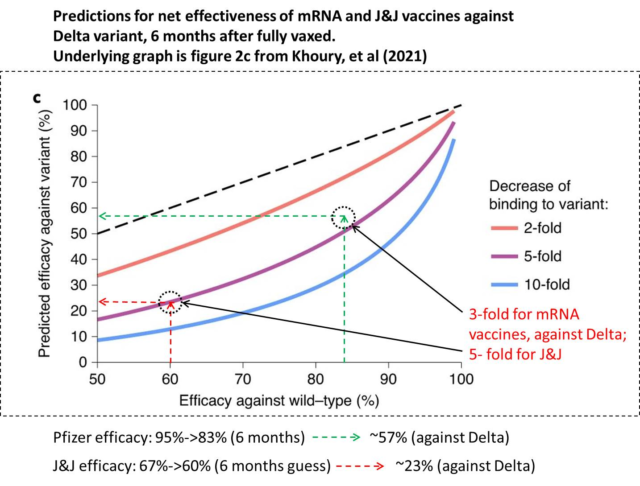
The authors also included figure 2c (at right), where it’s easier to read off the predicted reductions in efficacy, given various reductions (2x, 5x, 10x) in neutralizing titer. I haven’t seen any trial measurements for waning immunity of the Janssen vaccine; but if we use the Khoury model, over 6 months it will drop ~28 points from 67% to ~39%. Assuming that the reductions in efficacy from waning immunity and variant escape are independent, the combined predictions are shown by red dashed lines at right.
Summarizing, there is evidence that Delta’s vaccine escape properties reduce the average efficacy of the mRNA vaccines from 95% to 77%. If we also take waning immunity into account, the net mRNA efficacy against Delta would be more like 57% after 6 months. And note that with trial results showing Pfizer at 42% and Moderna at 76%, the average for mRNA vaccines is 59%, which puts the theoretical model very close to observed results. For the Janssen vaccine, the story is not good at all. After 6 months, the net efficacy for Janssen against Delta might be as low as 12% (based on my assumptions).
This analysis should give you an idea why the doctors at San Francisco General have started giving supplemental shots of Pfizer or Moderna to people who previously got the Janssen single shot vaccination. And why the CDC decided to change their guidance to masking fully vaccinated people at the end of July, and why the FDA is likely to greatly accelerate an Emergency Use Authorization (EUA) for booster shots, especially for previous Janssen recipients.
What’s It Take To Achieve Herd Immunity?
The classical formula for herd immunity says that you have to vaccinate (or have diseased and recovered) at least the critical fraction of the population, Vc , which is given by:
Vc = [(R0-1)/R0] / EV, where:
R0 is the reproduction number of the virus, and EV is the efficacy of the vaccine.
The CDC thinks that R0 for Delta is between 5 and 9. So for example, if we take the least transmissible value, R0 = 5, and suppose that an evolved version of the mRNA vaccines has EV = 90% against Delta, then: Vc = [(5-1)/5] / (0.9) = 0.889, and we have to vaccinate at least 89% of the population. For R0 = 7, the midpoint of the estimate for Delta transmissibility, Vc = 0.952 or 95.2% of the population. If we think the virus is more transmissible, at the upper end of the CDC’s range, with R0 = 9, then Vc = [(9-1)/9] / (0.9) = 0.988, and we have to vaccinate almost everyone, about 99% of the pop. This is guaranteed to be impossible without something approaching martial law. . .We did it for measles, but it took years to eradicate. These required coverage percentages imply we will still be passing the virus amongst ourselves for quite some time.
More From Gregg Dieguez ~ “InPerspective”

Mr. Dieguez is a native San Franciscan, longtime San Mateo County resident, and semi-retired entrepreneur who causes occasional controversy on the Coastside. He is a member of the MCC, but his opinions here are his own, and not those of the Council. He lives in Montara. He loves a productive dialog in search of shared understanding. >>
<< Mr. Laird is another semi-successful, semi-retired MIT entrepreneur but with more degrees, living in Los Altos. They roomed and caused trouble together back in the day. Bruce produces a periodic newsletter on the science and implications of COVID-19. For a free subscription, contact Bruce at: laird2007@hotmail.com